Oral Cancer Education
What is Oral Cancer?
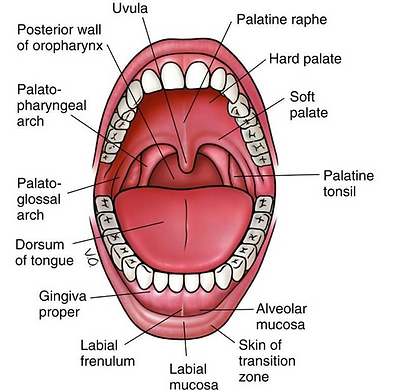
Oral cancer is a non-communicable disease. It is a type of cancer that occurs in the mouth (oral cavity), throat (oropharynx) and/or the lip.
Oral cancer occurs when the cells in the mouth (oral cavity), throat (oropharynx) and/or the lip grow and reproduce themselves in an uncontrolled manner. These cancerous body cells can invade and destroy healthy tissues (including organs) surrounding them or even far away from them, such as the cervical lymph nodes, lung, kidney, liver, bones, and breast.
Figure 1 shows the longitudinal view of the lip, mouth, and throat to give you a picture of these body structures where oral cancer can occur.
There are different types of oral cancer, and they include squamous cell carcinoma (which forms approximately 90% of oral cancer cases), sarcoma, lymphoma, and melanoma of oral structures.
According to the World Health Organization, oral cancer is the 13th most common cancer in the world. In 2020 alone, over 370,000 people were diagnosed with oral cancer while over 170,000 people died from it, majority of which are people in socially disadvantaged groups or regions.
Oral cancer is commoner in older age groups, and it kills more men than women because the risk factors of oral cancer are commoner in men than in women. However, more cases of (and deaths from) oral cancer are now being reported among women and younger people due to rising rate of oral cancer risk factors among them (please see Section B to learn more about the risk factors of oral cancer).
You can learn more about the meaning of oral cancer by clicking here
What are the Risk Factors of Oral Cancer?
Many factors have been identified to increase one’s risk of developing oral cancer. The most common risk factors include:
Major Risk Factors
-
The use of tobacco. Examples include smoked tobacco (cigarettes, cigars, shisha, pipe) and smokeless tobacco. Smokeless tobacco includes products such as chewing (spit) tobacco, moist snuff, snus (a “spitless,” moist powder tobacco, often in a pouch), and other tobacco-containing products that are not smoked.
-
Heavy drinking of alcoholic beverages. Examples of these beverages include wine, gin, rum, spirit.
-
The chewing of betel quid (a.k.a. gutkha or paan) or areca nut products (e.g. Babul, Beeda, and Mawa).
-
Oral infection by human papillomavirus (HPV). HPV is a virus that can be transmitted to the mouth through oral sex.
-
Consumption of diets low in vegetables and fruits. Examples of vegetables and fruits are bananas, citrus, spinach, apple.
Other Risk Factors
-
General health condition(s) that weaken(s) the body’s immune system. Examples of these conditions include HIV/AIDS, cancer, and the use of drugs that suppresses the immune system (e.g. in patients with organ transplant).
-
Some oral conditions that can lead to oral cancer. These conditions are called oral potentially malignant disorders. Three major examples of these conditions include leukoplakia, erythroplakia, and oral submucous fibrosis. Leukoplakia is a white patch while erythroplakia is a red patch. Both patches cannot be rubbed off from the oral cavity, and they can occur together in the mouth, forming erythroleukoplakia. On the other hand, oral submucous fibrosis is a hardening of the lining of the mouth, and it is also characterized with band formation in the mouth, whitening of the lip, restricted mouth opening, and burning sensation.
-
Having a family history of oral cancer.
-
Exposure to ultraviolet rays from the sun or artificial sources (e.g. tanning lamps). This can cause cancer of the lip.
-
Exposure to some industrial chemicals. Examples of these chemicals include asbestos, chlorinated solvents (e.g. chloroform, chlorinated alkenes, perchloroethylene, etc.), petroleum-based solvents (e.g. benzene, kerosene, gasoline, etc.), and oxygenated solvents (e.g. alcohol, diethyl ether, ethylene glycol, etc.)
-
Chronic trauma (or irritation) to the mouth. Recurrent and prolonged oral trauma (or irritation) may lead to oral cancer. Examples of such trauma includes trauma from sharp dentures, sharp teeth, and faulty implants.
-
Poor oral hygiene. Poor oral hygiene increases the risks of infectious oral diseases, which may ultimately progress to oral cancer.
People with exposure to two or more oral cancer risk factors are more likely to develop oral cancer in later life than those with one or no oral cancer risk factor.
However, it is also important to note that despite having oral cancer risk factors, some people may still not develop oral cancer in later life. Regardless, this should not encourage continual exposure to these risk factors.
You can learn more about the risk factors of oral cancer by clicking here
What are the Signs and Symptoms of Oral Cancer?
The sign and symptoms (that is, clinical features) of oral cancer can arise from any part of the mouth, the throat, and the lip. The most common clinical features include the following:
-
Ulcer in the mouth that lasts for more than three weeks.
-
White or red patch in the mouth.
-
Lump (exophytic growth) in the lip, mouth, throat, or neck.
-
Swallowing difficulty.
-
Unexplained bleeding in the mouth
-
Numbness in the mouth
-
Change or hoarseness in voice.
-
Pain or burning sensation in the mouth or throat.
-
Persistent swelling in the mouth
-
Sudden tooth mobility
-
Unintentional loss of body weight.
The figures (Figures A – D) are examples of oral ulcer, oral lump, white patch, and red patch seen in cases oral cancer.
In case you notice any of these features in your head and neck area, it is advisable to promptly contact your dentist for further advice.
You can learn more about the signs and symptoms of oral cancer by clicking here
You can click here to watch a video on the experience of an oral cancer survivor concerning the early signs and symptoms of the disease.




How can Oral Cancer be Prevented?
Oral cancer may be prevented from occurring. The following measures (ways) can be used to prevent it:
Avoidance of tobacco use:
Abstinence from both smoked and smokeless tobacco is a major way of preventing oral cancer.
However, for those who are already tobacco users, they can consider the option of quitting tobacco use.
You can quit tobacco use by enrolling in tobacco cessation programmes in a healthcare centre offering such services.
Avoidance of alcohol use:
Abstinence from all forms of heavy drinking of alcoholic beverage is another major way of preventing oral cancer.
According to the USA’s National Center for Chronic Disease Prevention and Health Promotion, heavy alcohol drinking is considered as drinking of fifteen or more alcoholic drinks on weekly basis for a man or eight or more alcoholic drinks on weekly basis for a woman.
Avoidance of the use of betel quid and areca nut:
Betel quid has three basic ingredients: areca nut, betel leaf, and slaked lime. The chewing of Betel quid, areca nuts, or related products can cause oral cancer. It is therefore advised that you avoid it. In a situation where you are addicted to its use, you can seek help from your doctor.
Avoidance of contact with hazardous industrial chemicals:
Avoid occupational exposure to industrial chemicals that can cause cancer. These chemicals include asbestos, chlorinated solvents (e.g. chloroform, chlorinated alkenes, perchloroethylene, etc.), petroleum-based solvents (e.g. benzene, kerosene, gasoline, etc.), and oxygenated solvents (e.g. alcohol, diethyl ether, ethylene glycol, etc.).
In a situation where your job involves contact with such chemicals, ensure to use personal protective equipment such as gas masks, protective gown, protective boots, etc.
Avoidance of unprotected oral sex:
Giving unprotected oral sex to your partner can increase your risk of contracting HPV. Therefore, it is advisable to use protective barriers when giving oral sex.
These barriers, when used correctly and regularly, can minimize your risk of contracting HPV.
Examples of these barriers include tongue condom, dental dam, and plastic wrap.
Vaccination against human papillomavirus (HPV):
HPV vaccination is a major way of preventing oral cancers caused by oral HPV infection.
HPV vaccine is very safe, and anybody aged 45 years or below should get themselves vaccinated against HPV.
You can contact your doctor to know if you are eligible to receive the vaccine.
Limiting exposure to ultraviolet (UV) rays from the sun:
UV rays can cause cancer of the lip. During outdoor activities, the use of wide-brimmed hat, and sunscreen and lip balm of sun protection factor of 30 or above can help to prevent such cancer.
Also, the UV from the sun is strongest at midday; hence, it is advisable you limit your outdoor activities during this period to protect yourself from oral cancer risks.
Oral cancer self-examination:
It is important you regularly examine yourself for the signs of oral cancer. This will help you in the early identification of oral cancer.
After examining yourself, you suspect that you have signs of oral cancer, please contact your doctor for advice.
Click here to watch a video on oral cancer self-examination:
Maintenance of healthy bodyweight and good dietary habits
Excessive body weight and poor nutrition has been linked to oral cancer.
Eating of more whole grains, vegetables and fruits is healthier.
Eat less of starchy foods and avoid or limit eating of red or processed meats, processed foods, and sugary beverages.
You can also fortify your food intake by taking vitamin supplements.
Maintenance of good oral hygiene
Poor oral hygiene increases the risk of infection in the mouth. Chronic infection can encourage the development and growth of oral cancer. Hence, good oral hygiene maintenance protects against oral cancer.
Regular dental check-ups:
Regular dental check-ups allow your dentist to examine your mouth and detect any oral health problems (including oral cancer) at the early stage.
Ensure to visit your dentist regularly.
You can learn more about how to prevent oral cancer by clicking here










How is Oral Cancer Diagnosed?
Early diagnosis of oral cancer is very advantageous, as it provides opportunity for early treatment interventions which curbs/minimises the risk of the spread of oral cancer to other parts of the body.
Oral cancer is primarily diagnosed through a biopsy. A biopsy is an examination of tissue removed from a living body to discover the presence, cause, or extent of a disease.
Biopsy is the most reliable way of diagnosing oral cancer. Because biopsy involves cutting out diseased tissues, this procedure is done under anaesthesia, making it a painless procedure.
There are different forms of biopsy. The two most reliable types of biopsies used for oral cancer diagnosis include the following:
Scalpel biopsy: A scalpel biopsy involves the use of a scalpel to remove a tissue suspected to have oral cancer together with a bit of surrounding normal tissue. Also, this procedure is the gold standard for oral cancer diagnosis. Please see Figure A below illustrating how a specimen is taken from the mouth during scalpel biopsy.
Punch biopsy: A punch biopsy involves the use of a punch biopsy forceps to remove a cylindrical specimen of oral tissue of between 0.4–0.8 mm in diameter from a suspected oral cancer site. The specimen obtained from procedure is smaller than that obtained from scalpel biopsy; hence, it is not as reliable as scalpel biopsy.
Asides the above major diagnostic techniques, several other adjunct techniques are also available. The two most common adjunct techniques are: (i) fine needle aspiration cytology (this involves the use of a needle to take suck out fluids and cells from the suspected oral cancer site), and (ii) vital staining of the suspected oral cancer site with a liquid called toluidine blue to detect the presence of oral cancer.
The adjunct techniques are usually less invasive but less reliable.
You can learn more about oral biopsies (the major oral cancer diagnostic techniques) by clicking here

How is Oral Cancer Treated?
Oral cancer is a curable disease, if detected early. Different options are available for the treatment of oral cancer. The treatment options of choice depend on many factors such as the size of the oral cancer, its location, if it has spread to other body parts, its genetic nature, and your age and general health conditions.
Depending on the situation, a single treatment modality or a combination of different treatment modalities can be used to treat oral cancer.
Below gives an overview of available treatment modalities:
Surgery:
This involves a surgeon operating on you to remove the oral cancer.
The surgery may also involve the removal of other nearby body parts (e.g. jaw, part of the tongue, lymph gland/node, etc.) if they have been affected by the cancer.
If a large body part is removed, a reconstruction surgery may be performed to rebuild the area.
Radiotherapy:
This involves the use of radiation to kill the cells of oral cancer in the body.
Radiotherapy can be given after surgery or if you are not able to undergo surgical operation, or to ease oral cancer symptoms if it has spread to other parts of the body.
Chemotherapy:
This involves the use of drugs that can kill oral cancer cells.
Chemotherapy can be given before or after surgery. Also, it can be given if oral cancer re-occurs or if it has spread to other parts of the body.
Targeted medicine and immunotherapy:
Targeted medicine involves the use of drugs that specifically target oral cancer cells.
Immunotherapy involves the use of drugs that will boost the body’s immune system’s capacity to kill oral cancer cells by itself.
Either of the above are used when oral cancer has spread to other parts of the body or when it re-occurs after treatment.
Finally, oral cancer can go away completely if it is treated early and adequately. Currently, over 80% of people that are treated of oral cancer when the disease was diagnosed early survived for at least five years after the diagnosis.
However, the chance of survival reduces when the disease is diagnosed lately (that is, when oral cancer has spread to other parts of the body). In this stage, oral cancer patients can benefit from palliative care to help them have a better quality of life.
It is also important to note that the treatment modalities for oral cancer have their associated risks, some of which include difficulty in eating, hair loss, dry mouth, alteration of cosmetic appearance of the face, and alteration of speech, among others. Hence, early diagnosis and treatment of oral cancer should not be delayed.
For all patients undergoing care for oral cancer, they may also benefit from supportive care (including psychological and spiritual care) services offered at their clinical care centres.
You can learn more about oral cancer treatment by clicking here




Do you need Support for Oral Cancer Care?
In case you feel that you need support concerning oral cancer, there are reputable charity organisations across the world that provide such support. These charity organisations do provide broad range of oral cancer-related care/support, including support for quitting habits that makes one to be at risk of oral cancer, mental and emotional support, as well as other forms of support within their scope of practice on oral cancer. Below are examples of such organizations and their online means of contact:
A) For people living in the United States of America:
Oral Cancer Foundation
Contact: https://oralcancerfoundation.org/contact/
Head and Neck Cancer Alliance
Contact: https://www.headandneck.org/contact-us/
B) For people living in the United Kingdom:
Mouth Cancer Foundation
Contact: https://www.mouthcancerfoundation.org
Swallows Head & Neck Cancer Support Charity
Contact: https://theswallows.org.uk/contact-us/
Macmillan Head and Neck Support Group
Contact: https://www.macmillan.org.uk/cancer-information-and-support/get-help
C) For people living in other countries
We would like to advise that you contact your local health authority for guidance on how to utilise an oral cancer support service in your area.
Support for Oral Cancer Care
Various organisations offer support for oral cancer patients and those at risk. Some reputable organisations include:
United States
United Kingdom
For those in other countries, please contact your local health authority for guidance on oral cancer support services in your area.
Our Sources of Information
The facts, images, and videos used in this educational content were obtained from the following sources:
Facts
-
Gov.UK. Chapter 6: Oral cancer [Internet]. Available from: https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention/chapter-6-oral-cancer. Published 09 November 2021. Accessed 01 October 2023.
-
NHS (National Health Service). Cancer [Internet]. Available from: https://www.nhs.uk/conditions/cancer/. Accessed 19 March 2024.
-
Cancer Research UK. Mouth and oropharyngeal cancer [Internet]. Available from: https://www.cancerresearchuk.org/about-cancer/mouth-cancer. Published 25 October 2021. Accessed 19 March 2024.
-
NHS (National Health Service). Mouth cancer [Internet]. Available from: https://www.nhs.uk/conditions/mouth-cancer/. Accessed 19 March 2024.
-
CDC (Centers for Disease Control and Prevention). HPV and oral cancer [Internet]. Available from: https://www.cdc.gov/oralhealth/fast-facts/oral-cancer-and-hpv-vaccine/index.html. Published 24 February 2022. Accessed 20 March 2024.
-
CDC (Centers for Disease Control and Prevention). HPV vaccine [Internet]. Available from: https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html. Published 16 August 2023. Accessed 20 March 2024.
-
American Cancer Society. Can oral cavity and oropharyngeal cancers be prevented? [Internet]. Available from: https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/prevention.html. Published 23 March 2021. Accessed 20 March 2024.
-
NCCDPHP (National Center for Chronic Disease Prevention and Health Promotion). Excessive alcohol use [Internet]. Available from: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/alcohol.htm. Published 11 July 2022. Accessed 20 March 2024.
-
CDC (Centers for Disease Control and Prevention). HPV and oropharyngeal cancer [Internet]. Available from: https://www.cdc.gov/cancer/hpv/basic_info/hpv_oropharyngeal.htm. Published 12 September 2023. Accessed 20 March 2024.
-
NHS (National Health Service). HPV vaccine [Internet]. Available from: https://www.nhs.uk/vaccinations/hpv-vaccine/. Published 01 September 2023. Accessed 20 March 2024.
-
NHS (National Health Service). Paan, bidi and shisha [internet]. Available from: https://www.nhs.uk/live-well/quit-smoking/paan-bidi-and-shisha-risks/. Published 31 October 2022. Accessed 22 March 2024.
-
CDC (Centers for Disease Control and Prevention). Head and neck cancers [Internet]. Available from: https://www.cdc.gov/cancer/headneck/index.htm. Published 28 June 2023. Accessed 22 March 2024.
-
NHS (National Health Service). Dental check-ups [internet]. Available from: https://www.nhs.uk/live-well/healthy-teeth-and-gums/dental-check-ups/. Published 17 January 2022. Accessed 22 March 2024.
-
NHS (National Health Service). Treatment for mouth cancer [Internet]. Available from: https://www.nhs.uk/conditions/mouth-cancer/treatment/. Published 19 June 2023. Accessed 22 March 2024.
-
WHO (World Health Organization). Oral health [internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health#:~:text=Oral%20cancer%20includes%20cancers%20of%20the%20lip%2C%20other,new%20cases%20and%20177%20757%20deaths%20in%202020. Published 14 March 2023. Accessed 11 June 2024.
-
Bagan J, Sarrion G, Jimenez Y. Oral cancer: clinical features. Oral Oncol. 2010 Jun;46(6):414-7. doi: 10.1016/j.oraloncology.2010.03.009. Epub 2010 Apr 18. PMID: 20400366.
-
Lewis MAO. Mouth cancer: presentation, detection and referral in primary dental care. Br Dent J. 2018 Nov 9;225(9):833-840. doi: 10.1038/sj.bdj.2018.931. PMID: 30412564.
-
Oliver RJ, Sloan P, Pemberton MN. Oral biopsies: methods and applications. Br Dent J. 2004 Mar 27;196(6):329-33; quiz 362. doi: 10.1038/sj.bdj.4811075. PMID: 15044984.
-
Sankaranarayanan R, Ramadas K, Amarasinghe H, et al. Oral Cancer: Prevention, Early Detection, and Treatment. In: Gelband H, Jha P, Sankaranarayanan R, et al., editors. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2015 Nov 1. Chapter 5. Available from: https://www.ncbi.nlm.nih.gov/books/NBK343649/ doi: 10.1596/978-1-4648-0349-9_ch5
-
Cirillo N, Duong PH, Er WT, Do CTN, De Silva MEH, Dong Y, Cheong SC, Sari EF, McCullough MJ, Zhang P, Prime SS. Are There Betel Quid Mixtures Less Harmful than Others? A Scoping Review of the Association between Different Betel Quid Ingredients and the Risk of Oral Submucous Fibrosis. Biomolecules. 2022 May 2;12(5):664. doi: 10.3390/biom12050664. PMID: 35625592; PMCID: PMC9138976.
-
Nikkilä R, Tolonen S, Salo T, Carpén T, Pukkala E, Mäkitie A. Occupational Etiology of Oropharyngeal Cancer: A Literature Review. Int J Environ Res Public Health. 2023 Nov 3;20(21):7020. doi: 10.3390/ijerph20217020. PMID: 37947576; PMCID: PMC10647348.
-
Barul C, Carton M, Radoï L, Menvielle G, Pilorget C, Woronoff AS, Stücker I, Luce D; ICARE study group. Occupational exposure to petroleum-based and oxygenated solvents and oral and oropharyngeal cancer risk in men: A population-based case-control study in France. Cancer Epidemiol. 2019 Apr;59:22-28. doi: 10.1016/j.canep.2019.01.005. Epub 2019 Jan 15. PMID: 30658217.
-
Christensen KY, Vizcaya D, Richardson H, Lavoué J, Aronson K, Siemiatycki J. Risk of selected cancers due to occupational exposure to chlorinated solvents in a case-control study in Montreal. J Occup Environ Med. 2013 Feb;55(2):198-208. doi: 10.1097/JOM.0b013e3182728eab. PMID: 23147555.
-
Mathur R, Singhavi HR, Malik A, Nair S, Chaturvedi P. Role of Poor Oral Hygiene in Causation of Oral Cancer-a Review of Literature. Indian J Surg Oncol. 2019 Mar;10(1):184-195. doi: 10.1007/s13193-018-0836-5. Epub 2018 Dec 7. PMID: 30948897; PMCID: PMC6414580.
-
Warnakulasuriya S, Kujan O, Aguirre-Urizar JM, Bagan JV, González-Moles MÁ, Kerr AR, Lodi G, Mello FW, Monteiro L, Ogden GR, Sloan P, Johnson NW. Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer. Oral Dis. 2021 Nov;27(8):1862-1880. doi: 10.1111/odi.13704. Epub 2020 Nov 26. PMID: 33128420.
-
Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024 May-Jun;74(3):229-263. doi: 10.3322/caac.21834. Epub 2024 Apr 4. PMID: 38572751.
-
Singhvi HR, Malik A, Chaturvedi P. The Role of Chronic Mucosal Trauma in Oral Cancer: A Review of Literature. Indian J Med Paediatr Oncol. 2017 Jan-Mar;38(1):44-50. doi: 10.4103/0971-5851.203510. PMID: 28469336; PMCID: PMC5398106.
Images
Courtesy of the images used in this educational content are given to the following sources:
-
American Celiac
-
Austin Radiation
-
Dubai Standard
-
EHS Daily Advisor
-
Getty Images
-
Hidoctor
-
Pixabay
-
Ruwan Jayasinghe (researcher)
-
Science Cell Online
-
The Guardian Nigeria
-
VectorStock
-
Your Perfect Smile
Videos
Courtesy of the videos used in this educational content are given to the following sources:
-
Mouth Cancer Foundation

